Prior authorization means getting approval before you can get access to medication or services. For services that require prior authorization or notifcation, be sure to call the member services number on the back of your health plan id card.
Seven Ways For Hospitals To Control Overhead Expenses - Healthmanagementorg
Some united health care now requires providers to obtain authorization for 60 minute therapy sessions.
United healthcare shared services prior authorization. The automated process will guide you through a series of questions, and review time may be faster. Box 25183 santa ana, ca 92799. We do not accept any out of state hmo plans.
Prior authorization and site of service review update; If the patient lives in delaware, florida, louisiana, maryland, north carolina,. Other united health care billing considerations.
You are responsible for obtaining prior authorization before you receive these services. Please contact your plan directly to receive authorization prior to being seen. All savers supplement united healthcare provider number;
If you have an hmo plan, please make sure that either dr. The health insurance portability and accountability act (hippa) protects your health information. Providers do not need to sign in to access information about authorizations/precertifications.
Risk adjustment data validation ; Notification/prior authorization is not required for emergency or urgent care. We focus on delivering customer solutions that meet their goals and strategies.
Braden is listed as your primary care physician or that you have an authorization from from your primary care physician to be seen at our office. Maximum 2 hearing aids every year; You can access the tool at uhcprovider.com/paan.
Sign in to link by clicking on the link button in the top right corner of uhcprovider.com, then select the prior authorization and notification app. Authorization is required for services after 36 visits. Shared services updates for geha
How does unitedhealthcare prior authorization? For more information, see the geha privacy policy. We work closely with brokers and clients to deliver custom benefits solutions.
At that point, hipaa or federal privacy laws may not protect your information. If you intend to see a client for longer than 45 minutes, you’ll want to obtain prior authorization to do so. Umr is a unitedhealthcare company.
Standard prior authorization request form please submit your request online using our prior authorization and notification tool on link. But, we can’t control what happens to your information after we share it with the person or organization you name on this form. Prior authorization requirement for synagis® and xolair® 01/2021:
Instructions on how/where to submit the completed form are included at the bottom of the form itself. Radiation therapy prior authorization update; More people turn to unitedhealthcare than any other company when it’s time to choose their medicare coverage.
Go to prior authorization and notification tool. Copayment for hearing aids $375.00 to $1425.00. (if you're ready to download an authorization forms, click authorization forms.) geha web accounts are protected from access by unauthorized users.
Optumrx prior authorization department p.o. It could be shared with others. Your employer pays the portion of your health care costs not paid by you.
Copayment for medicare covered benefits $0.00 copayment for routine hearing exams $0.00 maximum 1 visit every year; Prior authorization can be requested in the following ways: We have earned a reputation for successful health plan innovation.
The authorization forms on this page are for geha's hdhp, standard and high option plan members. Administrative services provided by united healthcare services, inc. Get help to find a plan.
Go to uhcprovider.com and click on the link button in the top right corner. Get medicare plans with more. This includes supporting member health and helping to interpret changes in the.
Click the authorization form you need to download it. During a peer to peer review, a unitedhealthcare clinical director will discuss the following with the physician and/or facility: Then, select the prior authorization and notification tool tile on your link dashboard.
Umr is not an insurance company. Unitedag's benefit trust (uabt) is the recognized leader in providing health care for agribusiness. Providers should fax physician progress notes and separate rehab notes with medical records (including cardiac history and recent cardiac events or procedures) to 816.257.3255.
Use the prior authorization and notification tool on link. You may also initiate your request by phone by calling the number on the back of the member’s health plan id card. Once you have obtained the authorization, please review it
Get health plans for you and your family, at every age and stage. © 2019 united healthcare services, inc. Prior authorization required for hearing exams hearing aids:
Medicare part d coverage determination request form (pdf) (387.51 kb) (for use by members and doctors/providers) for certain requests, you'll also need a.
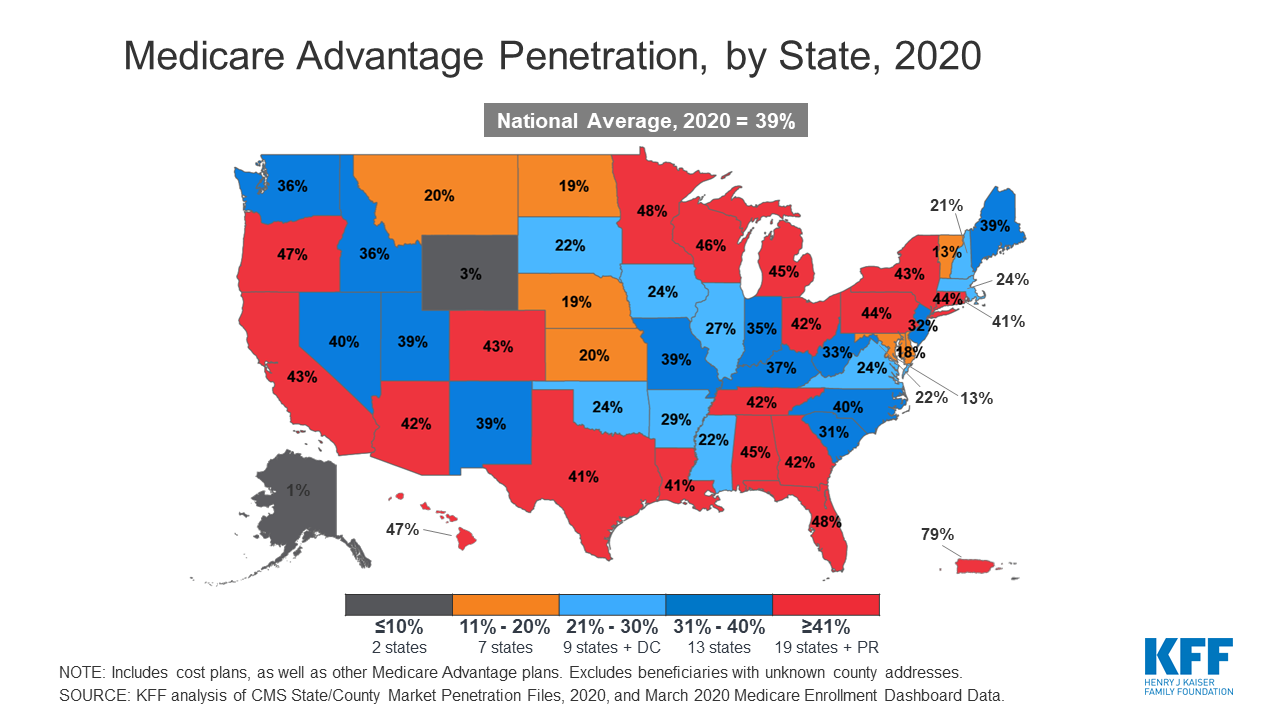
A Dozen Facts About Medicare Advantage In 2020 Kff

Ex-991 2 Ex99-1htm Therapeuticsmd Inc Presentation Dated August 2018 Therapeuticsmd
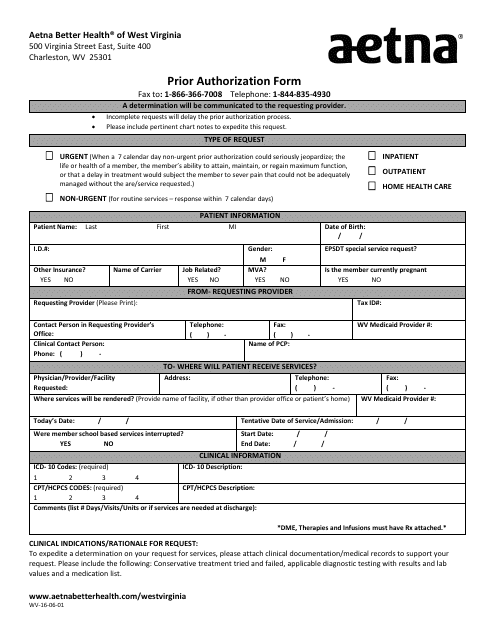
Business Forms And Templates Pdf Download Fill And Print For Free Templateroller
2
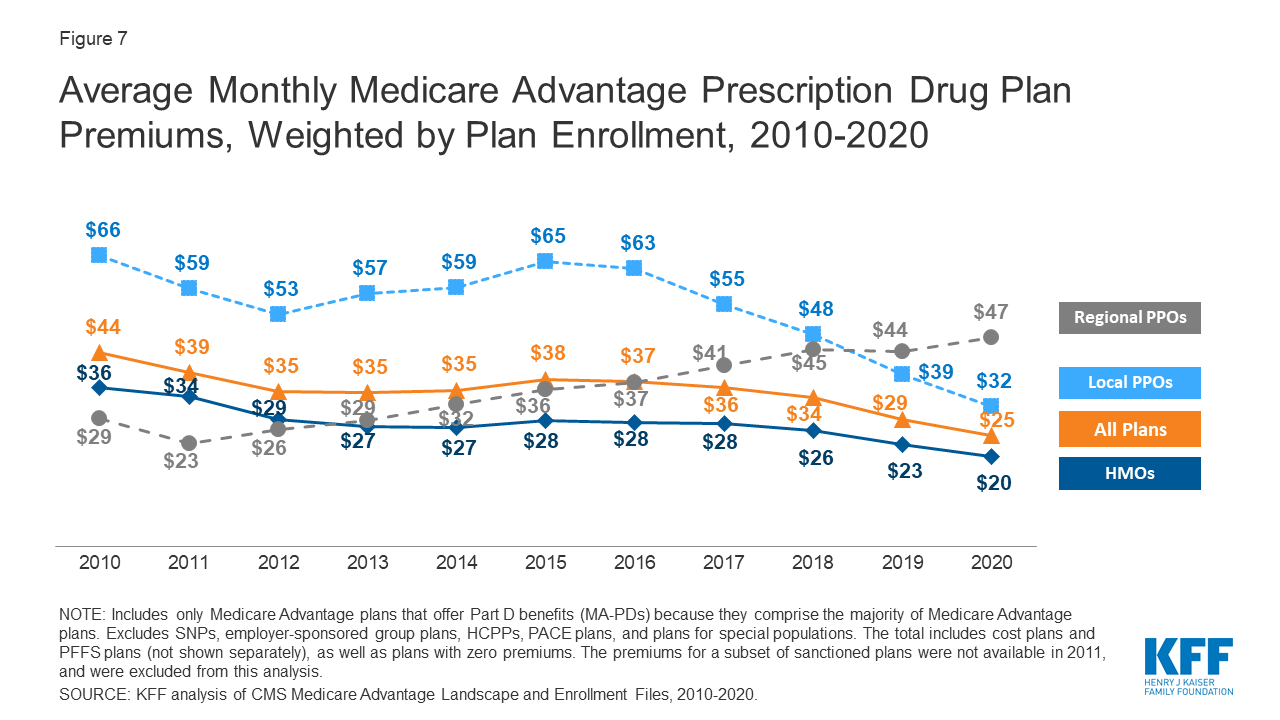
A Dozen Facts About Medicare Advantage In 2020 Kff
2

Sprouts Therapy
2
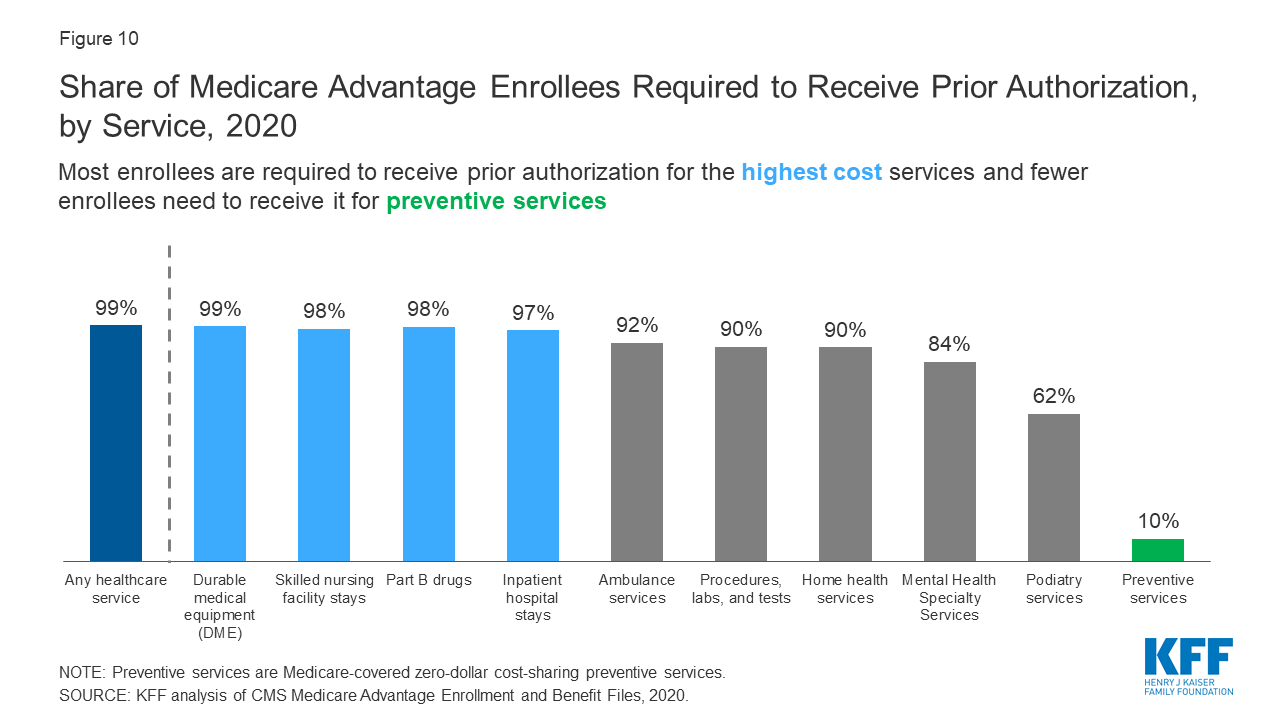
A Dozen Facts About Medicare Advantage In 2020 Kff

Sprouts Therapy
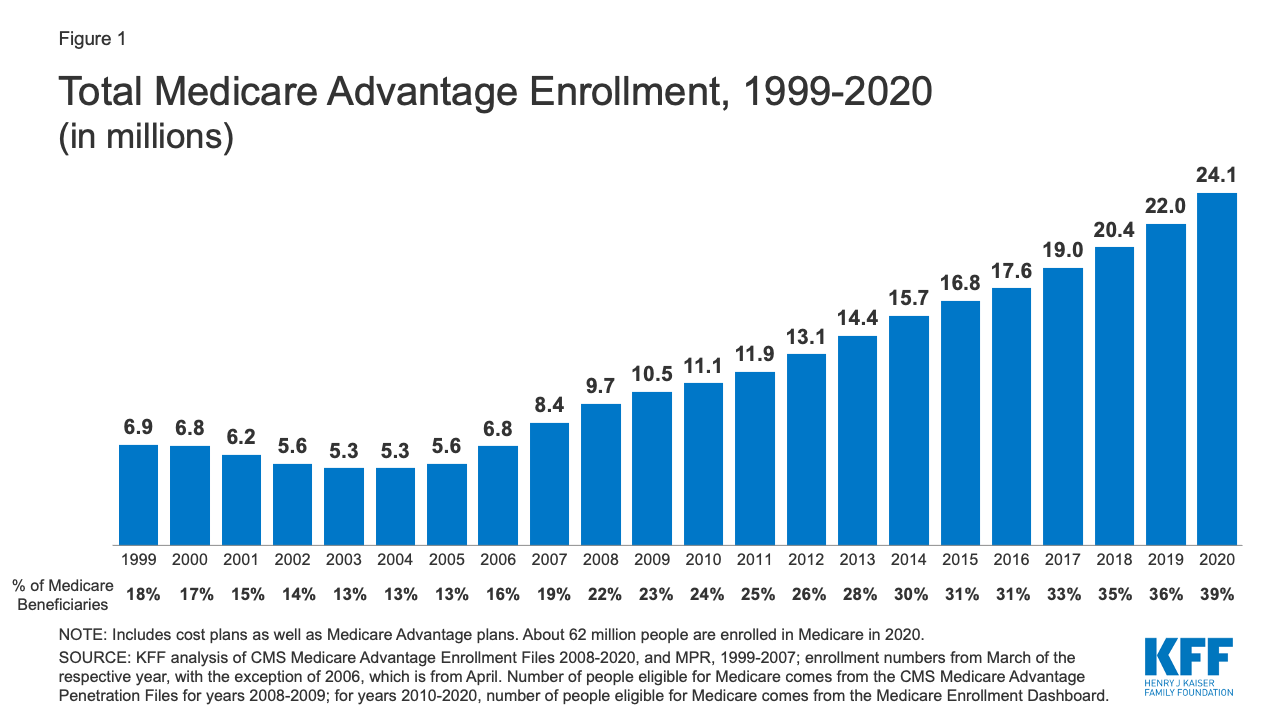
A Dozen Facts About Medicare Advantage In 2020 Kff
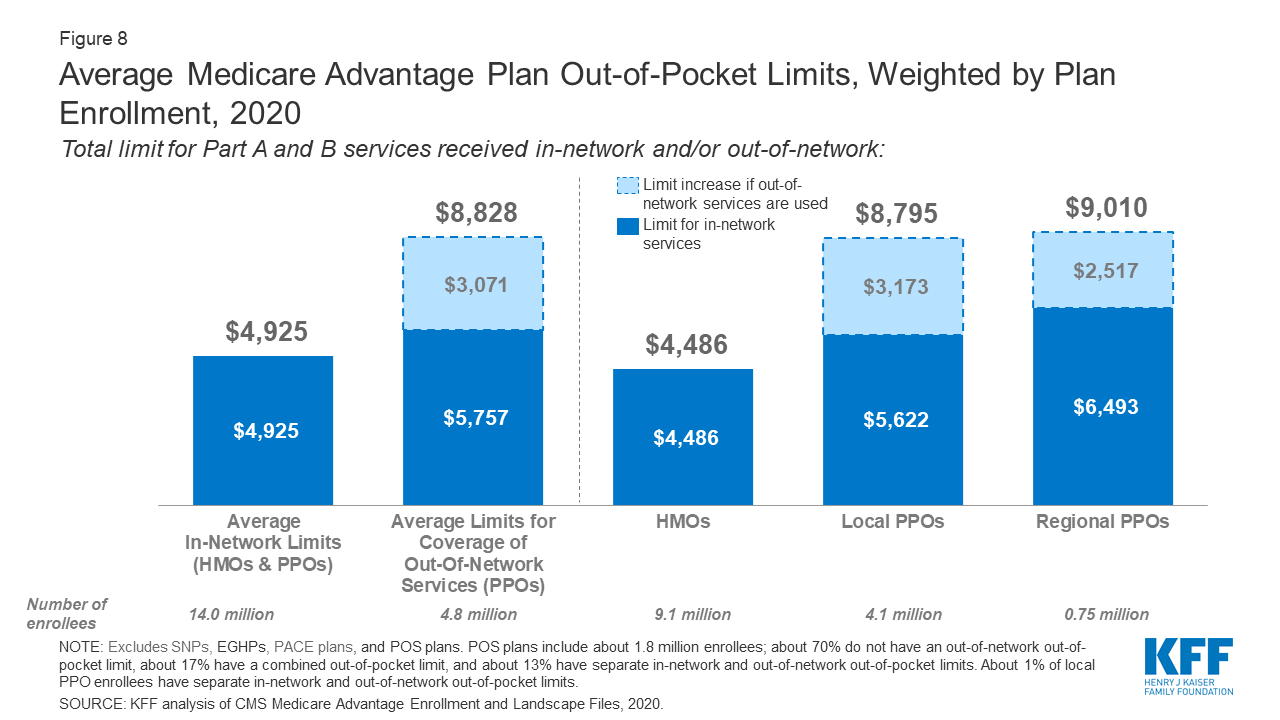
A Dozen Facts About Medicare Advantage In 2020 Kff
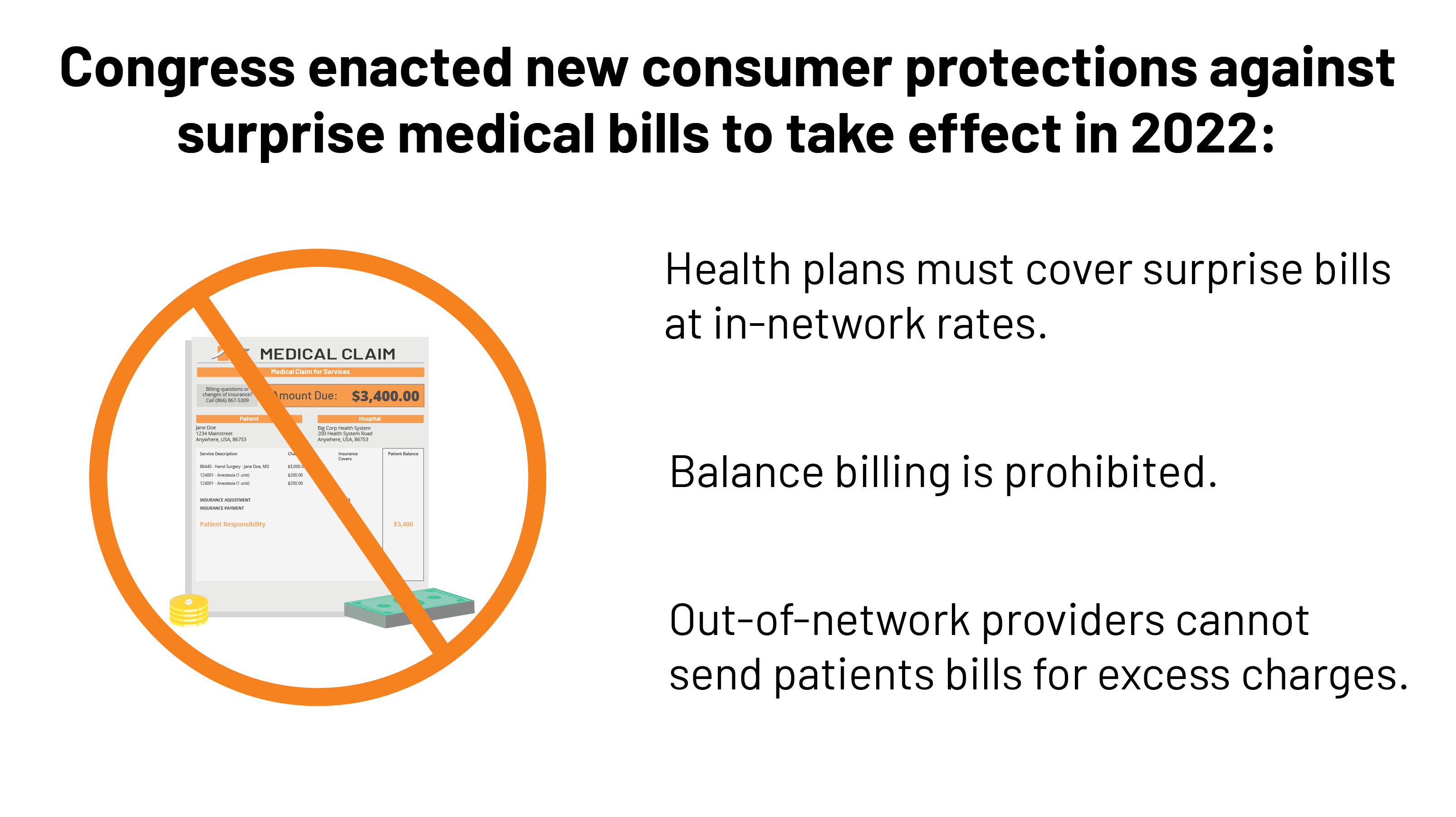
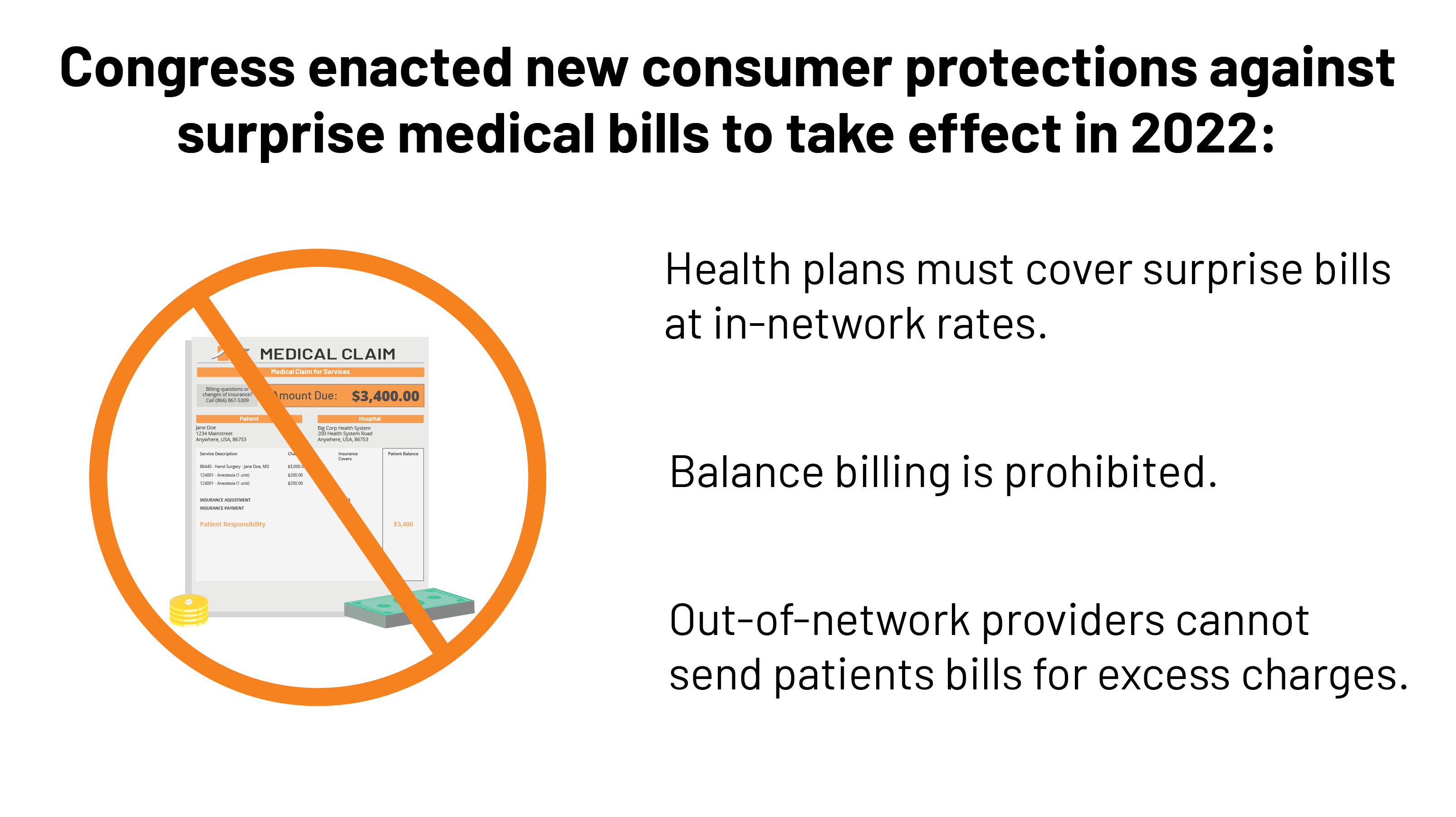
Surprise Medical Bills New Protections For Consumers Take Effect In 2022 Kff
Health Policy Flashcards Quizlet
2
Seven Ways For Hospitals To Control Overhead Expenses - Healthmanagementorg
2
Business Forms And Templates Pdf Download Fill And Print For Free Templateroller
Health Policy Flashcards Quizlet
Comments
Post a Comment